The Atlantic recently ran an article touting a new Commonwealth Fund study purporting to show that waiting to see a doctor is no big deal in European countries with “universal” health care systems.
The article concludes:
So much of the uproar over the recent insurance plan cancellation notices has been prompted by fears that the affected people will no longer be able to see the doctors they prefer or to get treated as quickly as they’d like. But compared to the rest of the Western world, that’s already the reality for many Americans. This report is just a sign that some countries have found a way to not only insure more people, but to get them the care they need faster.
Are you comforted? Sure, your health insurance may have been cancelled, but take heart – if you lived in the Netherlands or Norway, you’d be cool.
This is Commonwealth’s latest slam on all things American. They’ve been doing it for decades now and it is beyond tedious. American doctors suck. American insurance sucks. American hospitals suck. American politicians suck. Basically, the American people suck because they aren’t Norwegian or something. In fact, the only real sucking going on here is the Commonwealth Fund itself, which is still sucking off the teat of Stephen V. Harkness, one of the great tycoons of the 19th Century who made his money from J.D. Rockefeller’s Standard Oil Company.
It is remarkable how often the fortunes of great American industrialists are used after their deaths to disparage the country and the economic system that made their wealth possible.
Unfortunately, the Commonwealth Fund has a very long track record of cherry picking information to distort its own research to score political points. Some years ago, it conducted a survey of employer attitudes and trumpeted the results far and wide – 58 percent (as I recall the number) of Employers Support an Employer Mandate! Wow! Whodda thunk? It was only buried very deep in the back of the report that you could find out how they got that surprising result. Employers were given only two options – given a choice between a single payer and an employer mandate, which would they prefer?
Lazy reporters rarely read an entire report. They rely solely on the press release about it, or at most, glance at the executive summary. Hence, we get stories like The Atlantic’s.
In this case, almost every point in the Commonwealth Fund’s press release is similarly distorted. For example, they write –
In 2013, more than one-third (37%) of U.S. adults went without recommended care, did not see a doctor when they were sick, or failed to fill prescriptions because of costs, compared with as few as 4 percent to 6 percent in the United Kingdom and Sweden.
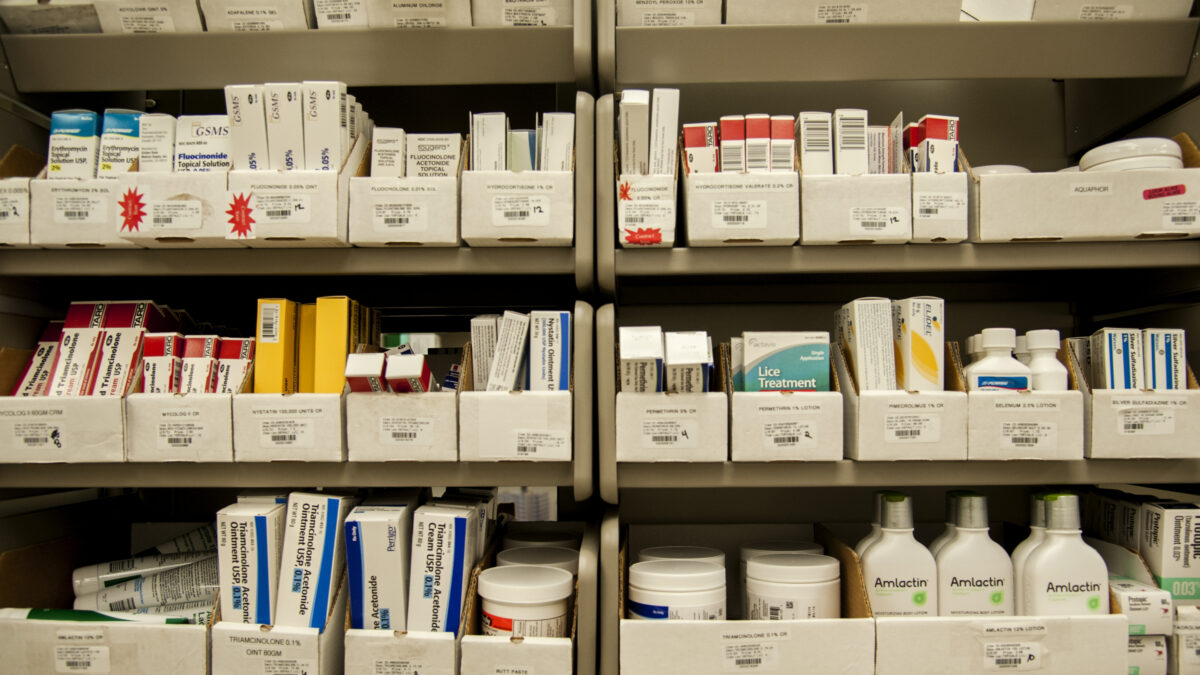
Note the clarifier. “because of costs.” They have nothing at all to say about people being denied care because of official rationing or lack of availability of services. Let’s concede that Americans may pay more to get, say, an MRI exam, but at least we can get it. In many countries there are so few MRI machines that people can’t get the test at any cost.
Roughly 40 percent of both insured and uninsured U.S. respondents spent $1,000 or more out-of-pocket during the year on medical care, not counting premiums. High deductibles and cost-sharing, along with no limits on out-of-pocket costs, may explain why even insured people in the U.S. struggled to afford needed health care, the researchers said.
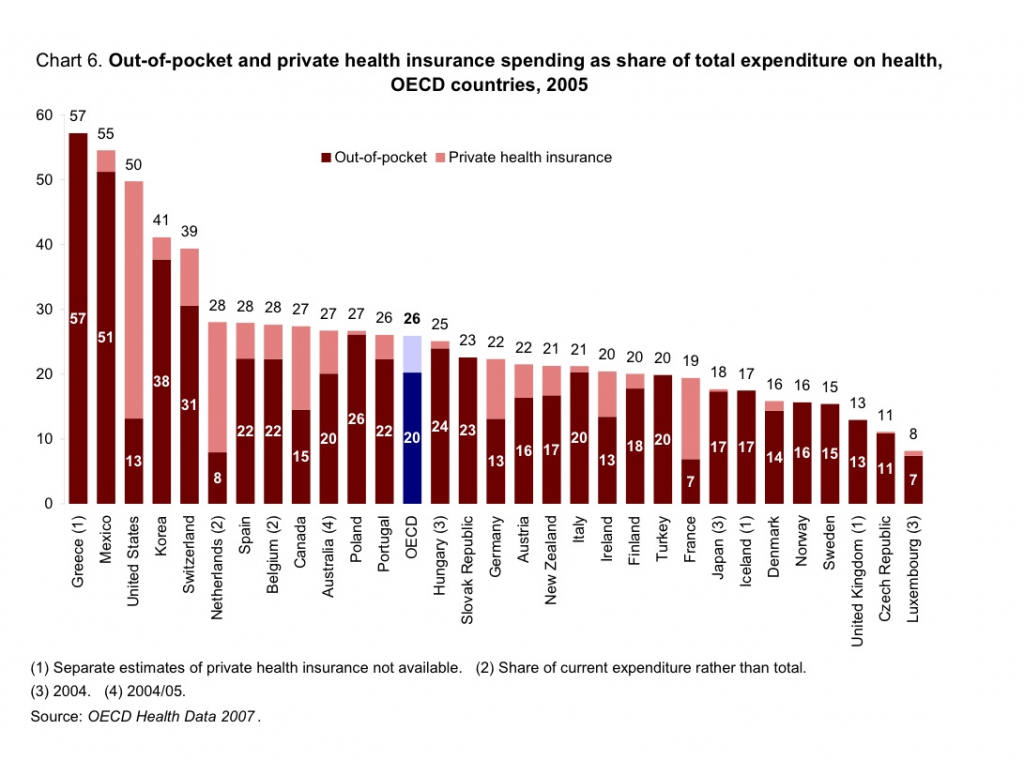
This is curious in a whole lot of ways. First, virtually every private plan does have a limit on out-of-pocket spending. The only major insurance plan that does not is the government’s own Medicare program. Further, the implication is that the United States is unique in requiring out-of-pocket payment. We are not. The OECD reports that, as a percentage of total health care spending, the United States has one of the lowest OOP responsibilities. (see below)
Nearly one-quarter (23 percent) of U.S. adults either had serious problems paying medical bills or were unable to pay them, compared with fewer than 13 percent of adults in the next-highest country, France, and 6 percent or fewer in the U.K., Sweden, and Norway.
Here, we have no way of knowing how they define “serious problems,” I’ve seen other research that identifies any discussion about costs with a doctor or any payment arrangements over time as a “financial burden” on patients.
About one of three (32 percent) U.S. adults spent a lot of time dealing with insurance paperwork and disputes or were either denied payment for a claim or paid less than expected. Only 25 percent of adults in Switzerland, 19 percent in the Netherlands, and 17 percent in Germany—all countries with competitive health insurance markets—reported these problems. U.S. insurers spent $606 per person on administrative costs, more than twice the amount in the next-highest country. Such high costs result from a complex, fragmented insurance system, the researchers write.
There is no question that insurance paperwork is a hassle, for both patients and providers, and it adds considerably to the cost of care. However, notice one sleight of hand here – they identify administrative costs as a dollar amount per person. Man. Talk about your shell game. Whenever there is a discussion of administrative costs for Medicare versus private insurance, it is always measured a percentage of claims – never on a per capita basis. Why would this be? Because Medicare claims are extraordinarily high, so even high per-person administrative expenses seem lower as a percent of the total. The Heritage Foundation conducted a study a while ago that found the per capita Medicare administrative cost was $509, while the per capita cost for private plans was $453. In the case of the Commonwealth report, half of the report is complaining how high American costs are compared to European countries, so if they reported admin costs as a percentage of total spending, it would seem much lower. Cynical? You bet.
But the biggest deception of all is this:
The vast majority (75 percent) of U.S. adults said their health system needs to undergo fundamental changes or be rebuilt completely.
This is supported in the “chart pack” by a chart illustrating the percentage of the population in 11 countries that say their own country’s health system “works well, only needs minor changes,” “needs fundamental change,” or “needs to be completely rebuilt.” Now, this is interesting because the lead author of this study, Cathy Schoen, has been involved in similar surveys for quite a few years. One was published in Health Affairs in 1999. At the time, they were surveying only five countries, all English speaking. Let’s compare those five countries in the 1999 to the same countries in this survey.
| 1999 | Only Minor Change | Fundamental Change | Completely Rebuilt |
| Aus | 19% | 49% | 30% |
| Can | 20 | 56 | 23 |
| NZ | 9 | 57 | 32 |
| UK | 25 | 58 | 13 |
| US | 17 | 46 | 33 |
| 2013 | Only Minor Change | Fundamental Change | Completely Rebuilt |
| Aus | 48% | 43% | 9% |
| Can | 41 | 50 | 9 |
| NZ | 47 | 45 | 8 |
| UK | 63 | 33 | 4 |
| US | 25 | 48 | 27 |
This is either the most astonishing turn-about in public opinion the world has ever seen, or the Commonwealth Fund is cooking the questions to get the desired results. How plausible is it that New Zealand went from 32 percent of the population saying their own system needs to be completely rebuilt to 8 percent in just 14 years? Not bloody likely. Curiously, Cathy Schoen is the only author involved in both studies.
I wonder if Mr. Harkness would be proud of how his money is being spent, or if he is rolling over in his grave today.